Understand
WHAT IS obstructive SLEEP APNEA - OSA?
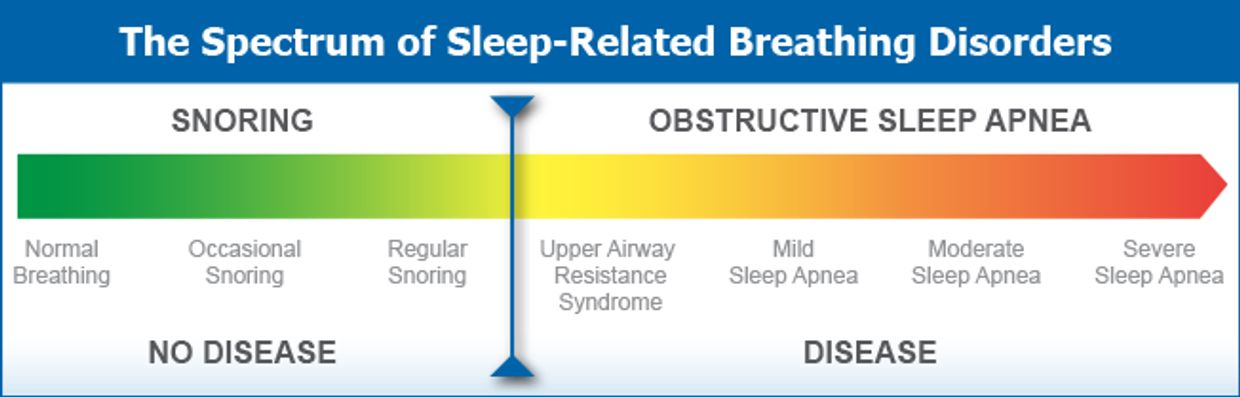
End state of SLEEP DISORDERED BREATHING
"Apnea," from Greek, means "without breath." Sleep apnea comes in three types: obstructive, central, and mixed. The most common is obstructive sleep apnea, often shortened to OSA.

TRADITIONAL TREATMENTS
They work to reduce the symptoms of Sleep apnea and they require a lifetime of intervention.
traditional treatment options
snoring appliance
managing sleep apnea
managing sleep apnea
- Nasal strips
- Snoring devices
- Laser treatments
managing sleep apnea
managing sleep apnea
managing sleep apnea
- C-PAP
- ORAL DEVICE - Mandibular advancement device
surgery
managing sleep apnea
surgery
- Upper airway stimulation (UAS)
- Uvulopalatopharyngoplasty (UPPP)
- Nasal surgery
- Maxillomandibular advancement surgery
prevent, treat and reverse sleep apnea

Vivos System
A significant advancement in sleep and airway medicine: A comprehensive treatment protocol for managing sleep-disordered breathing, including mild-to-moderate obstructive sleep apnea.
dangers of uncontrolled obstructive sleep apnea

high blood pressure
Sleep apnea can exacerbate high blood pressure. Frequent nighttime awakenings can trigger increased stress in the body, leading to overactive hormone systems and elevated blood pressure levels. Moreover, reduced oxygen levels in the blood due to breathing difficulties during sleep can further aggravate the condition.
For individuals with both sleep apnea and high blood pressure, a promising treatment approach involves integrating sleep apnea treatment with blood pressure medication. This combined approach is likely more effective in lowering both nighttime and daytime blood pressure levels compared to individual treatments alone. Ultimately, this may result in a significant reduction in cardiovascular risk.
cardiovacular disease and endothelial dysfunction
Obstructive Sleep Apnea (OSA) has been associated with endothelial dysfunction, potentially explaining the elevated risk of cardiovascular issues and overall mortality among affected individuals.
One plausible explanation for this dysfunction in OSA is the repetitive cycle of oxygen deprivation and re-oxygenation during episodes of interrupted breathing. This cycle disrupts the body's clotting mechanisms, diminishes the availability of nitric oxide, and promotes inflammatory and clot-forming processes. Additionally, the endothelium's capacity to repair itself and counteract increased damage is compromised. Collectively, these factors contribute to vascular problems, ultimately leading to adverse cardiovascular outcomes.
How are Depression and Sleep Related?
Depression and sleep issues often go hand in hand, with nearly everyone experiencing depression also having trouble sleeping. Doctors usually consider sleep problems when diagnosing depression.
This relationship between depression and sleep works both ways: poor sleep can lead to depression, and those with depression are more likely to have sleep troubles. Figuring out which came first, the sleep problems or the depression, can be challenging.
Common sleep problems linked to depression include trouble falling or staying asleep (insomnia), sleeping too much (hypersomnia), and obstructive sleep apnea. Insomnia is the most common, affecting about 75% of adults with depression. Around 20% have obstructive sleep apnea, and about 15% experience hypersomnia. Many people with depression may switch between insomnia and hypersomnia during the same depressive episode.
Sleep problems can contribute to depression by affecting the neurotransmitter serotonin and disrupting the body's stress system and circadian rhythms, making someone more likely to develop depression.
snoring
Mild, occasional snoring is generally considered normal and usually doesn't require medical attention. Its main impact is on the comfort of a bed partner or roommate who may occasionally be bothered by the noise.
However, frequent snoring (occurring more than three nights per week), known as primary snoring, can be more disruptive to bed partners but typically isn't a health concern unless it results in sleep disturbances or signs of sleep apnea. In such cases, diagnostic tests may be necessary.
Snoring associated with Obstructive Sleep Apnea (OSA) is more concerning for health. If left untreated, OSA can significantly affect sleep quality and overall health, leading to daytime drowsiness and being linked to serious conditions such as cardiovascular problems, high blood pressure, diabetes, stroke, and even depression.
Risk of motor vehicle accidents
Recent research has identified a concerning association between obstructive sleep apnea (OSA) and a significantly higher risk of motor vehicle accidents. Individuals with sleep apnea are nearly 2.5 times more likely to be involved in motor vehicle accidents as drivers compared to those without sleep apnea.
Moreover, further analysis of the risk factors linked to these accidents highlights that severe excessive daytime sleepiness, inadequate sleep duration of 5 hours or less, and the use of sleeping pills are independent predictors of increased crash risk among individuals with sleep apnea. These findings underscore the importance of addressing sleep apnea and related factors to enhance road safety.
Acid reflux / GERD and Sleep Apnea
Around 60 percent of individuals with sleep apnea also endure chronic acid reflux, known as gastroesophageal reflux disease (GERD). Acid reflux occurs when the lower esophageal sphincter remains open, allowing stomach acid to move back into the esophagus. Common symptoms of GERD include heartburn, chest pain, a sour taste in the mouth, and bad breath. However, it's possible to have GERD without noticeable symptoms.
There exists a significant link between obstructive sleep apnea (OSA) and acid reflux. Several studies have emphasized how OSA can worsen reflux, and vice versa. Research indicates that addressing OSA can ease reflux symptoms, while treating reflux can diminish the severity of OSA.
One possible explanation for this connection lies in the negative pressures created in the chest wall during apnea events. These pressures not only push acid but also bile, digestive enzymes, and bacteria upward. There have been documented instances of pepsin, a digestive enzyme, discovered in middle ear, sinus, and lung samples. This could potentially damage teeth, especially in mouth breathers with reduced saliva levels, which usually have alkaline properties.
Diabetes and Sleep Apnea
The connection between diabetes and sleep disorders, such as obstructive sleep apnea (OSA) and insomnia, is substantial:
- Approximately 72% of diabetes patients experience either OSA or insomnia.
- Up to 40% of individuals with OSA also have diabetes.
- A study found that 86% of obese patients with type 2 diabetes also had OSA.
- Abdominal or central obesity (an "apple shape") is a common risk factor for both type 2 diabetes and OSA.
- Independent research has shown that snoring is associated with a twofold increased risk of developing diabetes over a 10-year period.
The relationship between OSA and metabolic function is intricate:
- Several studies have established a link between OSA and insulin resistance and glucose intolerance, even when accounting for obesity.
- Research has also demonstrated a correlation between the severity of hypoxia (low oxygen levels due to apneas) and the extent of insulin resistance.
- Sleep deprivation studies have revealed an increase in glucose intolerance in otherwise healthy individuals.
The link between diabetes and OSA can be attributed to various factors, including:
- Drops in oxygen levels during apnea events.
- Inflammation of body tissues and cells.
- Reduced sleep duration and diminished sleep quality.
Understanding and addressing these connections between diabetes and sleep disorders is vital for comprehensive healthcare and disease management.
drrodrigues@chesterdentalcareva.com
Chester, Virginia